Can new payment methods in health system affect quality of care?


By Francisco Londono, August 10, 1998
Introduction
For the purpose of this article I will make some generalizations
and I will define some words to facilitate the reading and understanding.
These definitions are not intended to be exhaustive and must be understood
only in the context of this article.
In America health has had its own evolution, passing
from the personal relationship between a physician and a patient to a complex
system with many actors. As technology developed, on one hand, the costs
increased and patients or their families weren’t able to pay by themselves.
As a consequence, new payers, such as Government and employers appeared
in the health industry. But once again, one treatment could be so expensive,
that the resources of a small employer wouldn’t be enough to cover it,
and his business could get in financial risk. Consequently, the typical
insurers began to play their own role: The affiliation of large number
of people paying a fixed premium per person and period of time, regardless
the cost of the treatments needed by each of their affiliates. A
patient could choose the provider, pay the treatment by itself, and later
the insurer reimbursed him the cost of it. If the number of affiliates
is high, the probability of a high cost treatment becomes more standard
or predictable and the excess of money the insurer earns with people who
pay and don’t get sick can absorb its costs. This is known as the “big
numbers” law.
On the other hand, physicians became more specialized,
and needed more technology not affordable on an individual basis. Now we
have physicians, nurses, hospices, clinics, hospitals and complex systems
joining all them in order to provide the care needed by patients. For the
purpose of this article I’ll call all of them providers.
Cost continued increasing, the relations between
these actors continued changing, and the characteristics of each of them
too. In the side of the insurers, in the 1980’s, the Health Maintenance
Organizations or HMO’s appeared. Despite their differences, in the beginning
most had similar characteristics: they were non-profit organizations providing
care to their affiliates with a selected net of providers and special rules
and procedures that patients and providers should follow in order to accept
the service and pay the provider.
Recently, in the search to achieve the key objective
of cost containment, the payment systems used have also changed. At the
beginning, the predominant way used by payers and insurers to pay providers
was a fee for each service they provided to a patient (fee for service
– FFS). The fees were defined sometimes by the provider, sometimes by the
buyer and other times by a negotiation between them. FFS payment system
had implied an economic incentive to providers in the form of being paid
more as more services were delivered to patients. Different efforts were
made to discourage the excessive cost. One of the best known, and still
in use, is the Diagnostic Related Groups (DRG's), where the provider received
a fixed amount of money for the complete care of a patient with certain
diagnose, despite the resources used in the care of the patient.
This helped, but was not enough.
Recent changes show that Medicare, to reduce its
expenditures, is shifting toward the affiliation of more people to health
care organizations (HMO’s). Medicare is paying HMO’s with a fixed amount
of money per person and period of time (per capita), equivalent to 95%
of the average cost of a Medicaid patient, instead of paying providers
directly. In this way Medicare could decrease its expenditures by 5%.
At the same time, in order to keep their costs down,
HMO’s are using new payment methods too. In addition to the traditional
FFS and DRG systems, they are sometimes paying providers in a per capita
mode, assigning a group of providers a group of affiliates and paying them
a percentage of the premiums collected from the affiliates. Sometimes they
only make contracts for some services so the per capita payment is rated
according to the scope of the services contracted. Other times, HMO’s give
economic incentives to reduce referrals, prescriptions or expensive treatments
to patients. If the total expenses of one group of affiliates exceed an
HMO established quantity, the providers are penalized and receive less
money or if they expend less than expected, they are better paid. The principal
arguments of the HMO’s to do so are: first, costs must be reduced, which
is generally accepted; second, the physicians are the critical decision
makers in term of costs, so they should have strong (economic) incentives
to reduce them; and third, it has been proven that many services are not
always necessary or are not cost-effective. Even though not all HMO’s are
the same, and not all of them use these kind of payment systems, I’ll use
the term of HMO’s in this article to refer only those who have these practices.
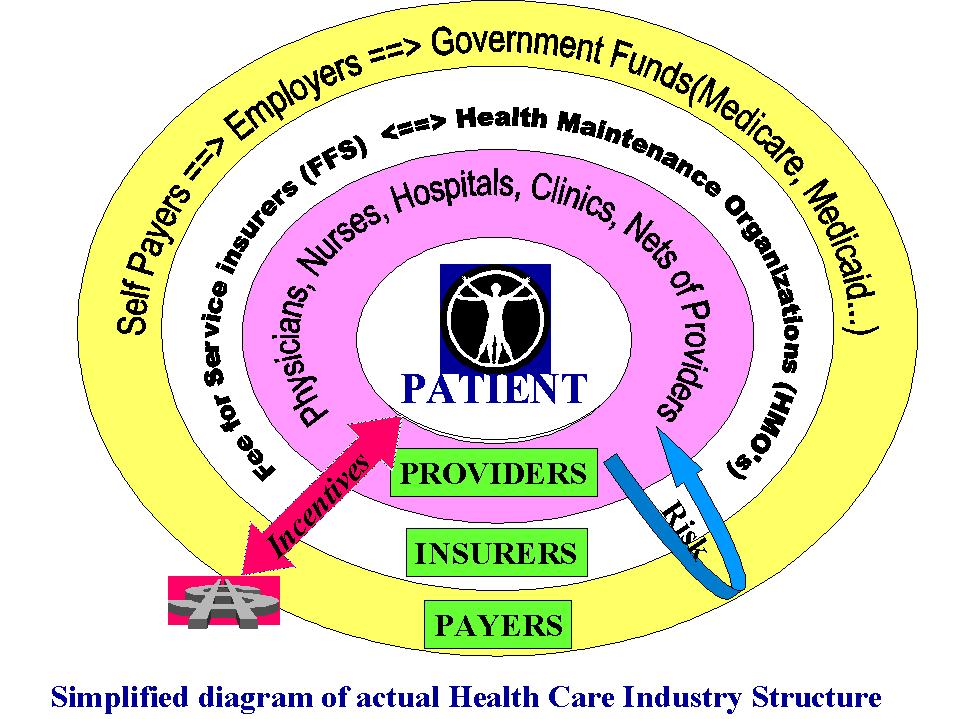
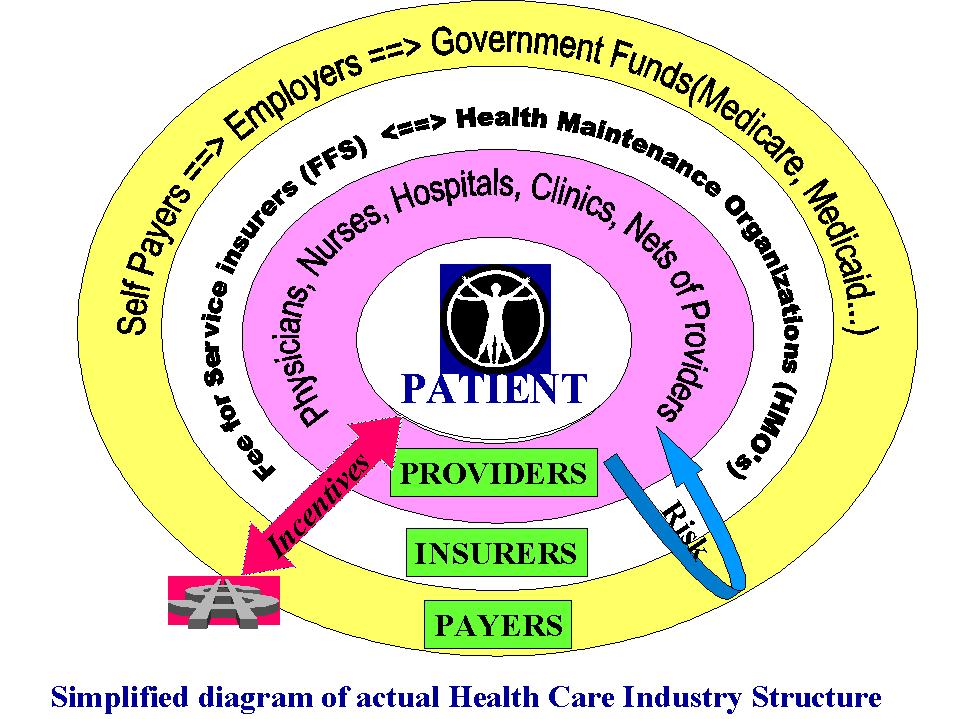
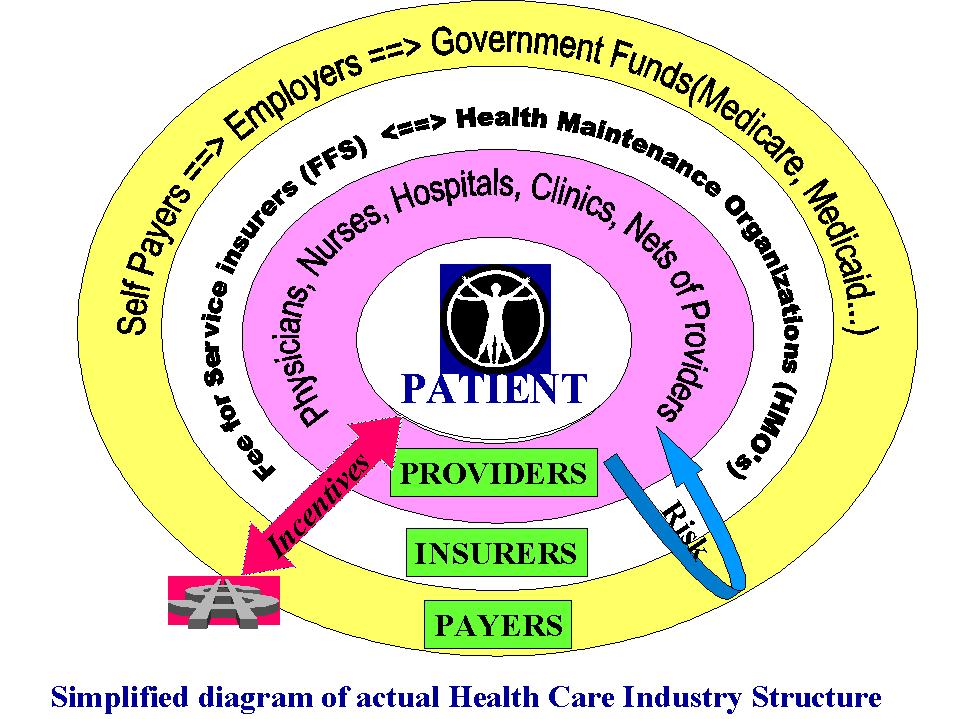
Next you will find a simplified diagram that depicts
how all this actors are integrated in a real more complex system than that
old one of the patient and his physician:
Principal questions about costs and quality implications
The purpose of this article is to analyze if these changes can affect the
costs and quality of care delivered to patients. Not all aspects of costs
and quality will be covered but some of the principal questions that have
emerged, some of the findings that have been done in the USA by some researchers,
and some conclusions will be given. The principal questions are:
? Are these new payment systems really helping to reduce costs?
? Whose costs are they helping to reduce?
? Do they affect the quality? How can they affect it?
? Are these new payment systems shifting the risk from the HMO’s to the
providers?
? Must we ask and answer ethical questions about incentives and similar
issues?
? Do different approaches exist to find a solution that helps to reduce
costs without affecting quality of care?
According to the importance of each question, all of
them will be addressed in turn.
Are these new payment systems really helping to reduce costs?
As the key objective of the new changes is cost control,
we must ask if the objective is being reached. Some findings directly related
to these new trends, show that they can really do it. A few of these findings
are:
-
For employers and self insurance buyers, it has been found that the rate
of increase in health care spending premiums has fallen from numbers higher
than 17% per year between 1987-1990 to near 2% per year between 1994-1996
(Hellinger, 1998). These findings show that at least the costs are not
growing higher than inflation as they usually did.
-
In his conclusions, Hellinger (1998:841) says “A recent review concluded
that the financial incentives for physicians are a key reason that managed
care plans have successfully reduced the use of health care services”.
-
Medicare is increasing the so called at risk contracts with HMOs at a fee
that represents 95% of the average Medicare spending per patient. This
new practice should help to reduce the cost of Medicare expenditures by
5%.
Whose costs are they helping to reduce?
As we saw in the last question, in many cases employers
and self-payers are finding savings or at least slow increments in their
premiums. Some researchers have found that the 5% cost reduction expected
by Medicaid is not going to happen. The principal reason for that conclusion
is that in some cases, HMOs are doing favorable selection to enroll healthier
people (Policy Information Exchange Online-PIE, 1996). In other terms,
even though is forbidden to reject the admission of a Medicaid beneficiary
in an HMO plan, they are targeting their marketing strategies toward healthier
people, such as younger people with good income. Bruce C. Vladeck, the
Health Care Financing Administration's (HFCA) Administrator commenting
on the study ‘Health Status of Medicare HMO Enrollees in 1994’ done by
the HFCA, said “This study clearly shows there still may be a problem of
risk HMO’s having healthier Medicare beneficiaries.” Later he also said
“These findings confirm again the need for a payment method that adjust
for the health status of Medicare beneficiaries who enroll in HMO’s.” (PIE,
1996). So, is Medicare going to save money this way? Probably not, because
the care for sicker people, and thus people more expensive to care for,
is still being paid directly to providers in a fee for service (FFS) way,
and their particular average cost must be higher. So, healthier people
costing Medicare 95% of actual expending average, and sicker people costing
more than the average, could make Medicare total cost rise. As Salins says,
HMO’s are “skimming the cream”. In this way, the HMO’s can keep costs down
the average and make profits. It is also known that some HMO’s have been
changed from no-profit to for-profit organizations.
Do they affect the quality? How can they affect it?
A primary question is how can these new ways of relationships,
with economic incentives to providers to control costs, affect the quality
of care? Before answering, a new question must be asked: What is quality
of care? There is no unique definition, but most authors recently included
in their definition aspects that not only concern the medical act itself,
but also the patient ease of access to the services needed and the general
satisfaction expressed by the patient itself. For the purpose of these
article I’ll only analyze these two factors.
Research has been done recently on this topic and
there is not enough evidence to have definitive conclusions (Hellinger,
1998:840). But some clues have appeared. As one critical aspect of quality
is ease of access, we must answer these questions: Is accessing in HMO’s
easier than that in typical insurers? Are the HMO’s accepting or denying
treatments recommended from providers to their patients? Can patients use
their preferred provider? In his revision of recent studies about ease
of access to care, Hellinger (1998:838) shows these findings:
-
Davis et al, 1995. “Enrollees in HMO’s were not as satisfied and had more
problems with access than enrollees in FFS (29% in HMO and 38% in FFS rated
plan as excellent; 26% in HMO’s and 45% in FFS rate access to specialty
care as excellent).”
-
National Research Corporation, 1996. “Enrollees in HMO’s had poorer access;
the percentage of enrollees in HMO’s who had no access problems (20.1%)
was less than for FFS (32.7%).”
-
Donelan et al, 1994. “Enrollees in managed care plans had poorer access.”
-
Brown et al, 1993, and Brown et al, 1993. “Medicare beneficiaries enrolled
in HMO’s were less satisfied and had poorer access than Medicare enrolled
in FFS.”
-
Nelson et al, 1996. “Medicare beneficiaries enrolled in HMO’s were more
than 3 times as likely to report access problems than Medicare beneficiaries
enrolled in FFS.”
Simultaneously, in recent years, as a response to the
increasing dissatisfaction and public claims about bad practice, more regulation
than ever has been made at state and federal levels, trying to protect
the people’s rights in access and quality of care (Dickerson, 1998). Laws
have been made to disclose the financial incentives that HMO’s offer physicians
to control costs, to give consumers the rights to a full appeal process
if denied treatment, to allow access to emergency-room care without previous
acceptance by the HMO, to grant minimum lengths of stay in hospital for
some treatments, to grant the continuity of plans from one HMO to another,
and so on.
As another clear answer to the permanent claims,
and a way to help people to choose between the different options, the Consumer
Assessment of Health Plans Survey (CAPHPS) is being developed. This study
is sponsored by the Agency for Health Care Policy and Research (AHCPR),
the Harvard Medical School, RAND, and the Research Triangle Institute.
In this survey nearly 130,000 people are being asked about their own experience
with different HMO’s or FFS plans. People are going to score their service
in many ways, but the research will take time and the results are expected
in November 1998 (AHCPR, 1998).
Are these new payment systems shifting the risk from the HMO’s to the providers?
Another problem that providers complain about, is that
with the per capita payment system and with the reimbursement based in
an inverse relation to the cost of the attention provided (economic incentives
to reduce costs), HMO’s are trying to shift the risk directly to the provider.
As explained in the introduction, one of the key principles of insurance
is the general law of “big numbers”. A patient’s treatment can be
so expensive that it can consume the resources of many patients. If the
group of patients is small, all patients’ premiums can be consumed and
the HMO or the provider loses money. If the group is large enough, then
the looses are much smaller. In general, providers joined in nets or alone
don’t have the same number of patients, and their risk is higher than that
of the HMO’s. As Salins says, shifting the risk to the providers, HMO’s
play a zero-sum game. They can assure profits and minimize almost to zero
the risk of looses. In his article, Salins also suggests that as providers
are taking risks, they are also beginning to do favorable selection. Some
teaching hospitals that typically have searched for the sickest people
in order to learn more are beginning to express their worries, because
if they continue doing the same way, and are being paid with the new systems,
they will no longer be able to cover their costs. So, who is going to care
for the sicker people? Once a provider or group of providers has over passed
in cost the reimbursement, who is going to pay for the services still needed
by patients? Can the provider absorb looses or are they going to refuse
treatments or services in order to survive? If the risk is going to be
shifted to the provider why do we need insurers, and of course why do we
need more actors to be paid in the chain of the health care industry?
Must we ask and answer ethical questions about incentives and similar issues?
Another key issue, very difficult to be studied with
numbers is the ethic question that physicians and providers have to ask
themselves frequently. What is first, the health of the patient or my income?
The answer seems very clear in the perspective of ethics, but what about
this other related questions: Is the prescription really needed? Are there
better options? Are better options more expensive? Are there other cheaper
options? Do they have the same risks? Are cheaper options well tolerated
by the patient? What level of treatment tolerance by the patient is desirable?
What is the right definition of cost effectiveness? What is the tolerable
level of effectiveness that a treatment must have in order to be accepted?
Is the use of pain control treatment worth it on a terminal person? and
so on. As medicine and health care are still not exact sciences, and the
concept of health is not unique and universal, many questions do not have
a clear answer, but providers have to make decisions on a day to day basis,
now.
Do different approaches exist to find a solution that helps to reduce costs
without affecting quality of care?
One of the best contributions that the HMO’s, the insurers
and the providers can make is just in progress, and all of them are working
hard to find “best practices” on health care. The information that can
be gathered today is not still completely used as it should be. Best practices,
if managed well, can help simultaneously to improve quality and reduce
costs. Health is not the exception to one of the principles of quality:
Quality costs less. We must not expect an exact answer to treat each different
illness in each patient, but Pareto’s law also applies to health. Most
costs are consumed delivering care to patients with a few common diseases
(Pareto’s law says < 20%). If we learn to treat well these few diseases,
we can increase quality and reduce costs. New studies of what is called
Evidence Based Medicine are in progress and they are going to help to decide
what treatments are the most indicated for the most important diseases.
Simultaneously with the support of the HCFA, new
approaches combining the FFS payment system with the Group-Specific Volume
Performance Standards (GVPS) are in progress. This new approach takes advantage
of giving economic incentives to providers based on quality of care and
the use of standards instead of using direct cost reduction incentives.
This approach would permit patients the freedom to choose the provider.
Also the providers could be paid on a FFS basis and be encouraged to use
cost-effective service delivery patterns (Tompkins et al, 1998).
Conclusions
According to the findings, accepting that the evidence
is not as complete as anyone should desire, and taking into account the
questions that are being made, some conclusions are:
-
More research is urgently needed in all these topics. Current research
studies and their findings are not enough. Sometimes this kind of research
is as complex and time consuming, that when the results are available things
have already changed. Although we can learn which things were done
good, which were not, which are the risks involved, and which must not
be repeated. Once you forget history you repeat the same mistakes.
-
Economic incentives to the providers are very dangerous in the field of
health. They can promote either over-treatment to increase providers’ benefits
or deny care needed to increase HMO’s profits. Many ethical questions have
to be asked and answered.
-
While incentives exist as they do today, effective controls must be designed.
Politicians, control agencies and all the health industry actors should
develop new laws to protect patient rights and prevent abuses. They are
not going to be perfect and there is no unique solution, but we have to
act right now.
-
The health market is known as an imperfect market, and the principal reason
is the information available to the actors. So, it’s important to support
the Consumer Assessment of Health Plans Survey (CAHPS, 1998). This will
help users to make a more reasonable and informed decision.
-
Hybrid approaches combining the use of information, GVPS standards and
FFS payment system must be encouraged strongly.
Finally it’s clear that the evidence available it is
still not enough to make definitive conclusions. However life is going
on, decisions are being made and must be made. Just with the scarce information
available today we have to make the right decisions, trying to decrease
the risks involved, and at the same time answering, in the most acceptable
way, the questions that have emerged.
BIBLIOGRAPHY
Agency for Health Care Policy and Research (AHCPR). (1997).
Consumer assessment of health plans (CAHPS): Fact sheet.
Available: http://www.ahcpr.gov:80/qual/cahpfact.htm. [1998, 16 July]
Dickerson, John. (1998). Lets play doctor. Time, 152 (2), 28-32.
Hellinger, Fred. (1998). The effect of managed care on quality: A review
of recent evidence.
Archieves of Internal Medicine, 158, 833-841.
PIE Online. (1996). Medicare risk HMOs experiencing favorable selection.
Available: htto://mimh.edu/TM/e26304T3777. [1998,7 July].
Tomkins, C; Wallace, S.; Bhalotra, S.; Chilingerian, J.; Glavin, P.;
Ritter, G &
Hodgkin, D. (1996). Bringing managed care incentives to Medicare’s
fee-for-service
sector. Health Care Financing Review, 17 (4), 43-63.
Salins, Craig. The new faces of “Managed Care.” Available:
http://www.peak.org/~ramselj/salinxx.txt. [1998, 2 July].